Warning: This article contains graphic descriptions of bodily mutilation.
Early in 2022, I wrote a piece for The Prindle Post discussing the arrest of John Yalu for the suspected murder of Kalman Tal. The circumstances surrounding Tal’s death are unclear, but the initial facts appeared to indicate that he had paid Yalu to amputate his leg, despite Yalu having no medical training. Speculation was, and remains, that Tal suffered from Body Integrity Dysphoria (BID), a rare disorder which makes sufferers feel like a disabled person trapped within a non-disabled person’s body and for which there is no agreed-upon treatment.
In that article, I argue that if we are committed to the principle of do no harm, then all treatment avenues, regardless of how distasteful we may find them, must be considered. Failing to do so would abandon those with the disorder to their suffering and force them to consider dangerous, even life-threatening alternatives like black-market surgery or DIY operations.
Fast forward to May 2024 and London, where the criminal court sentenced Marius Gustavson, 46, to prison. Charged with, amongst other things, five counts of causing grievous bodily harm, Gustavson was given a life sentence, meaning he will serve no less than 22 years behind bars. The actions that warranted such a severe sentence have a Hannibal Lecter quality.
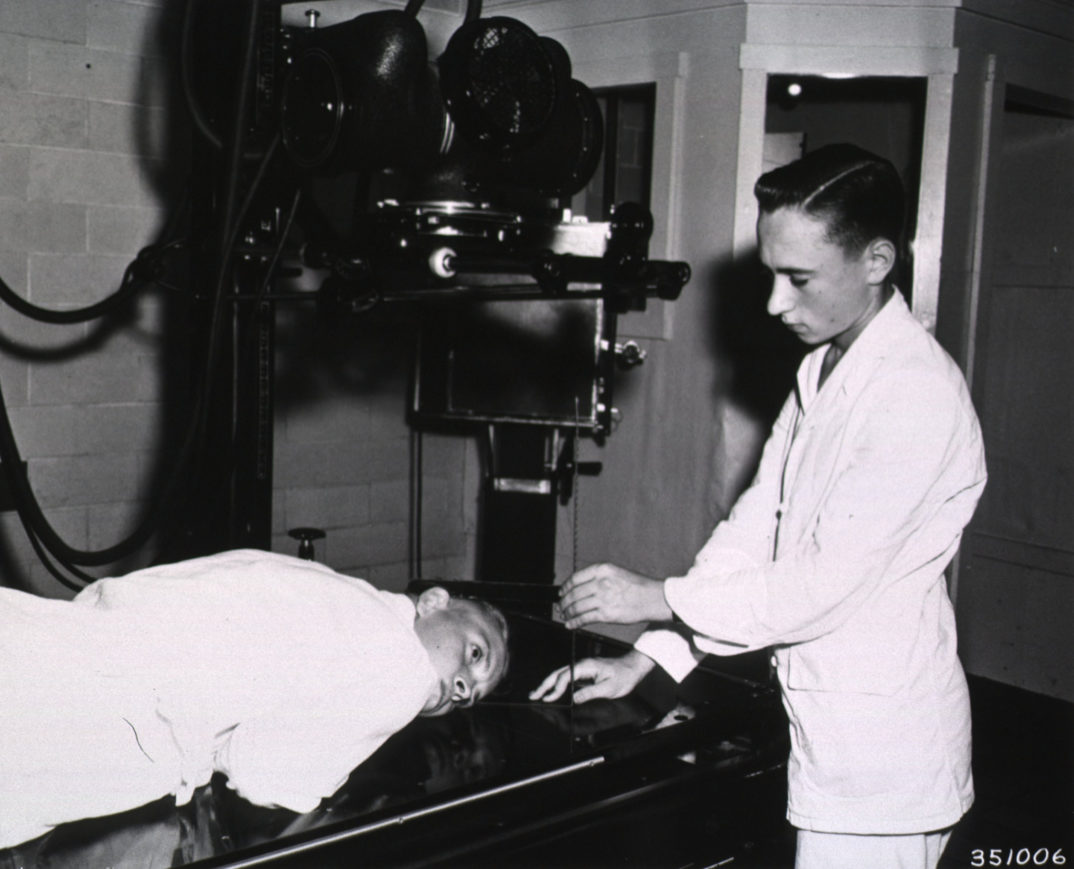
Gustavson, who called himself the “eunuch maker,” ran a highly profitable business providing body modifications to willing participants. This was despite neither Gustavson nor any of those assisting him having medical training. Additionally, these operations were carried out in non-surgical settings as seemingly innocuous as flats and hotel rooms. This, by itself, would be shocking, but it is not simply that operations were carried out by criminally unqualified individuals such as Gustavson. What elevates this into the realm of body horror is the operation’s nature, severity, and voyeurism.
As listed by the Criminal Prosecution Service, the 22 procedures in which Gustavson was involved included “the removal of the victims’ testicles, the amputation of penises, clamping of testicles with burdizzo clips (ordinarily used by vets in the castration of cattle), and the insertion of needles into genitalia.” It was not simply that these bodily parts were removed or mutilated, although that is itself horrifying, but that such tissue was then kept by Gustavson and his accomplices either as trophies, to be sold online, or in what might be the most disturbing fact of this case, to be cooked by Gustavson and ate.
To add another layer of horror to this case, Gustavson not only carried out these procedures but also ran a pay-per-view service where subscribers could watch him work. Altogether, between 2017 and 2021, Gustavson’s business earned him £223,229.43, $32,972.99 and €24,799 in profit.
What links this to the Yalu and Tal case is that Gustavson claims to have been suffering from BID. What’s more than this is that, according to his legal defense, Gustavson wanted to put “a smile on people’s faces by offering a service to those suffering, like him, from what was described as [BID].”
Now, whether Gustavson suffered from BID is a matter for debate. He had undergone surgical interventions himself to alter his physicality. This included, but is not limited to, having his penis removed in 2017 in a procedure carried out in a London flat and, in 2019, had to have his leg amputated after he deliberately submerged it in dry ice. Those who helped Gustavson in both instances also received jail sentences.
For my part, I doubt whether he had BID. His actions do not conform with the symptoms typically associated with the disorder. Most notably, those with BID rarely seek additional amputations or modifications once the part of their body which caused the initial distress has been removed. Gustavson, on the other hand, sought multiple modifications. Additionally, his desire appears to have begun to manifest after his divorce in 2016. Those with BID start experiencing symptoms in mid to late childhood. So, I suspect Gusatvson was using BID as a legal defense to lessen the likelihood or severity of his criminal sentencing. This did not work.
But, why does this matter from a philosophical and ethical standpoint?
First, it draws into question what the purpose of medicine is and what procedures fall under the umbrella of treatment. We typically accept that the amputation of a diseased limb to save someone’s life is acceptable. But is that the only circumstance? Might it be those other motivations, such as body modification or the improvement of the quality of life, could justify limb amputation?
Second, there are questions of justice and resource allocation. Who should pay for these operations and the ongoing support for the “willingly” disabled? Is it OK to amputate a limb if the individual pays out of pocket? What about access to benefits and social support? Should these be assigned to those who could have otherwise not needed them?
Third, we face questions about the limit of consent. Can you provide valid consent to such an operation, or are there certain things to which you cannot consent? Does this even matter in the case of such surgeries?
And fourth, can these interventions be legal? Is there any way that such an operation can be justified within the eyes of the law, or is the law’s very purpose to prevent such harmful acts, like these, from occurring?
But what I think both Gustavson and Yalu’s cases raise is the vulnerability of those suffering from BID. Those with the disorder have nowhere to turn to address the significant distress that they experience, which can last for decades, even entire lifetimes.
If the purpose of medical practice is to use knowledge of science and biology to improve the quality and length of life, then it seems clear that this will involve, in some exceptional circumstances, interventions which may be ethically troubling and socially distasteful. Indeed, many of the interventions and technologies which we might today consider ethically untroublesome or even mandated, like organ donation, were once viewed as affronts to the sanctity of the body and to nature itself.
This is to be expected as new knowledge and technologies extend the sphere of medical practice into realms which, for one reason or another, had previously remained outside its control.
Resisting calls to even investigate the effectiveness of amputation in BID cases cuts off potential treatment options for those with the disorder. This, in turn, means that those with BID feel betrayed, unseen, or misunderstood by the medical profession. So, they seek out alternative treatments, making them easily exploitable by the likes of Gustavson, who conducted these “surgeries” not to provide any therapeutic benefit but to satisfy his own desires and to make money.
It may be weird. It may be unbelievable. But until a better alternative comes along, amputations conducted under proper surgical conditions may be the best way to help those with BID. After all, who is likely to cause more harm, a trained surgical professional working with the proper tools in the right environment or someone like Gustavson, selling the spectacle of quasi-surgery and eating what he takes?