What is “obesity”?
The answer you’ll find in medical textbooks is simple. Divide one’s weight in kilograms by the square of their height in meters: if the answer is over 30, then they meet criteria for obesity. But as is always the case, the joints of reality are not cleanly carved by a single equation in a textbook: the reality of obesity, and the depth of the question at hand, is much more complex.
In the clinical setting, obesity is often thought of as a disease. But even if we assume that we have a good grasp on what a disease is, there is significant resistance to thinking of obesity as one: some argue that such a claim ignores personal responsibility and encourages unhealthy behavior, while others argue that thinking of obesity as a disease stigmatizes the people who live with it and further propagates the discrimination which they already face in our society. Others argue that obesity isn’t a disease, but a risk factor: they point out that obesity is associated with conditions classically understood as diseases, such as diabetes or hypertension, but it is not a disease per se. Still others argue that the medicalization of obesity is, in and of itself, a mistake: that akin to a disability, defining obesity as a risk factor or a disease is pathologizing a mere difference in the human experience.
This year, The Lancet, a highly respected medical journal, convened a commission composed of 60 expert clinicians and scientists to tackle these questions. The answers they consider to these questions warrant our attention, whether we are clinicians, philosophers, or laypeople. The Commission on the Definition and Diagnosis of Clinical Obesity takes an approach with a clinical tilt but a deeply philosophical history, and reveal something important about the words we use and the ways in which we use them: preliminary reports are that the commission didn’t just turn to the science to answer these very difficult questions, but sought to change the questions themselves.
* * *
The philosopher David Chalmers defines conceptual engineering, as a first pass, as “the process of designing, implementing, and evaluating concepts.”
Chalmers uses the example of a bridge – a structure designed to serve a particular purpose. Plans are implemented, the bridge is built, and, over time, the bridge is assessed for any faults which have developed. Conceptual engineering is much of the same, but with words instead of bridges. Take a word which I’ve spent time thinking about: harm. Philosophers write papers designing concepts of harm, often with a particular purpose in mind (whether it be resolving wrongful-life lawsuits or the non-identity problem). Those concepts are then implemented, whether theoretically or in practice, the results are assessed, and improvements are designed and implemented. This is a very common pattern in philosophy, with metaphysics being applied to practical philosophy and ethical practice.
But conceptual engineering is not just something for philosophy journals: in everyday life, concepts radically shape our political and social environments. Take the concept of “citizen”: the question of who is and is not a citizen has fundamentally shaped political life for centuries, and still does. Think of the most saliently divisive political conflicts of the modern day. In most cases, the fundamental disagreement revolves around the definition of basic concepts (life, gender, etc.).
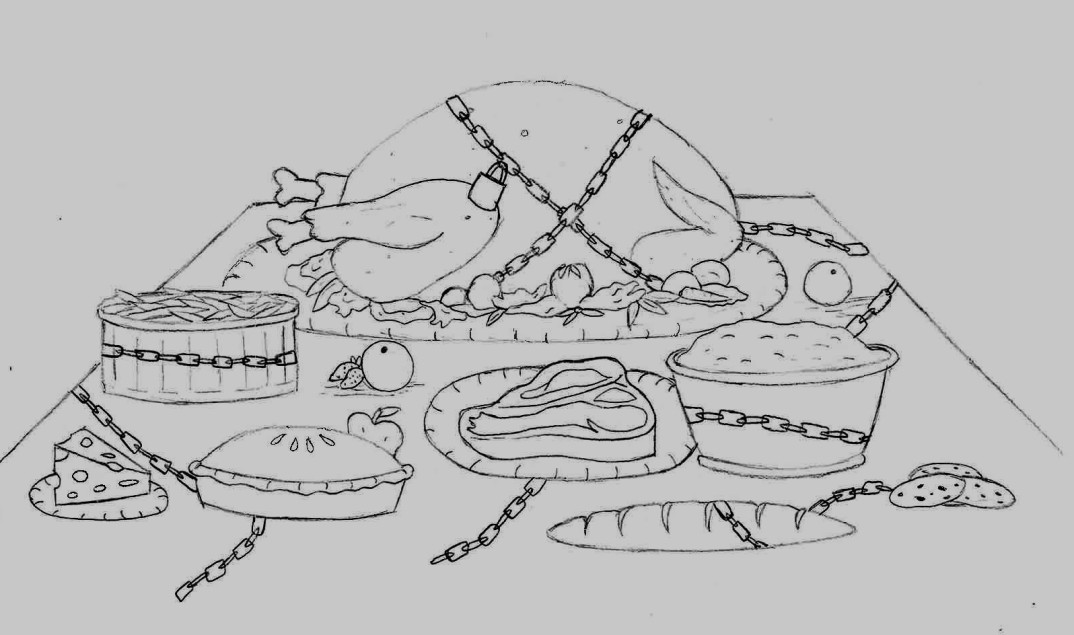
Though perhaps less obvious in everyday discourse, the concept of obesity is no different. Current projections are that 1.4 billion adults will be living with obesity by 2035, with a global economic impact of $4.32 trillion in the same year. 30 years of research has shown that healthcare providers are implicitly biased against people living with obesity. The relationship between stigma, obesity, and poor mental health outcomes has been extensively documented, especially in children. Understanding this concept is not just important for medical practice, but for our society as a whole.
The Lancet’s commission was convened exactly for this reason. Interestingly, their stated approach was to redefine obesity. In an interview with MedScape, Dr. Francesco Rubino, the project lead, said: “renaming ‘obesity’ is very important. The word is so stigmatized, with so much misunderstanding and misperception, some might say the only solution is to change the name.” He notes, further, that the commission focused on the concept of “clinical obesity” rather than obesity more generally, noting how the two may differ in the same way the concepts of “depression” and “clinical depression” might differ. By establishing a definition, then, Rubino and the commission hope to improve access to care and reduce stigma.
As of writing, the commission has not yet released their final report. But the approach that Rubino and the commission intend to take is clear: that of the conceptual engineer. The WHO recognized obesity as a disease 80 years ago, and that concept has been implemented over the intervening time. We see very clearly, though, that there are cracks in the foundation. The concept of obesity has become wrapped up in stigma, doesn’t reliably track a state of disease, and has proven ineffective in guiding research and clinical management. Rubino and his colleagues, just like the engineer who assesses the bridge, have found the foundation lacking, and seek to change the concept of obesity to better serve our purposes.
We shouldn’t lose track, however, of the important insight which can be found here. Concepts are tools which humans use, and often define. In the philosopher’s vocabulary, obesity is not a natural kind: obesity, rather, is a concept designed by humans for human reasons. Charitably, physicians seek to help people live fulfilling lives, and obesity may impede human thriving; more realistically, physicians have pathologized a group of people who already experience discrimination within and beyond healthcare. Seeing this reality, Rubino and his colleagues have hinted at a moral argument for changing the definition of obesity: the concept of obesity propagates harm and is ineffective at producing human good, and, therefore, we should consider changing it.
Many concepts which we encounter in our daily lives can be analyzed in this way: they are human inventions with human intentions and human faults, and we can redraw the lines of these concepts for moral reasons. We decide what our words mean, and, in most cases, the concepts which we rely on can be changed to make the world a better place, whether our concerns be utilitarian or deontological. Our concepts were designed to serve us, and when they fail to fulfill their role, we should ask if they might be changed for the better.